Outcomes of Craniectomy to Relieve ICP
In one study in the New England Journal of Medicine, researchers, led by Peter J. Hutchinson, Ph.D., F.R.C.S., looked at the outcomes of people who undergo the surgical procedure craniectomy to lessen intracranial pressure (ICP) due to traumatic brain injury.
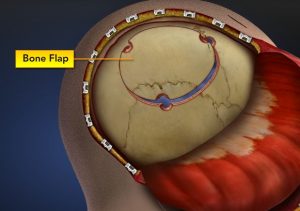
A craniectomy involves removing a bone flap to reduce intracranial pressure.
A craniectomy involves a surgical procedure where a portion of the skull is removed to relieve pressure on the brain. A craniectomy removes a bone flap, but the flap does not get replaced at the end of the procedure, unlike a craniotomy. The purpose of the procedure is to reduce intracranial pressure. The bone flap may be replaced in a second procedure, but artificial bone or plates may also be used. Some of the complications of the procedure may include seizures and pain, which can be managed with medication. For more on craniotomy and craniectomy, view this page: https://chicagobraindamage.com/craniotomy-craniectomy-essential-brain-surgery/
The group who underwent craniectomy to relieve intracranial pressure had a lower mortality rate than those who had their intracranial pressure managed medically without surgery.
Despite lower mortality rates, the surgery group had higher rates of vegetative state than the medical group. The surgical group also had higher rates of lower severe disability and upper severe disability than the medical care group. Rates of moderate disability and good recovery were similar in the two groups.
So, this means that people who undergo craniectomy to relieve pressure on the brain have less chance of death, but greater chance of being in a vegetative state, or otherwise being dependent on others to care for them.
This new information needs to be part of the discussion that doctors have with patients’ surrogates. “The findings of this trial argue for more investigation into the nuances of selecting patients for decompressive craniectomy after traumatic brain injury and for the development of more refined clinical decision-making tools,” writes Lori A. Shutter, M.D., and Shelly D. Timmons, M.D., Ph.D. in an editorial about the study in the New England Journal of Medicine. “Quality of life is an individual determination, and it is important to engage patients’ surrogates in discussions that focus on the patients’ previously stated wishes and personal values.”
Included in the discussion should be “potential outcomes of therapeutic options, prolonged recovery times, and the expected quality of life after neurologic injury.”
This entire study raises the question of whether or not quality of life is more important than life itself. The surgical group had higher rates of dependency on others, but lower rates of mortality. The question is complex, and the answer to it may depend on individual situations.